IBUS: Why are we focusing on these areas?
Too Little, Too Late: Targeting early, high quality antenatal care (ANC) in pregnancy
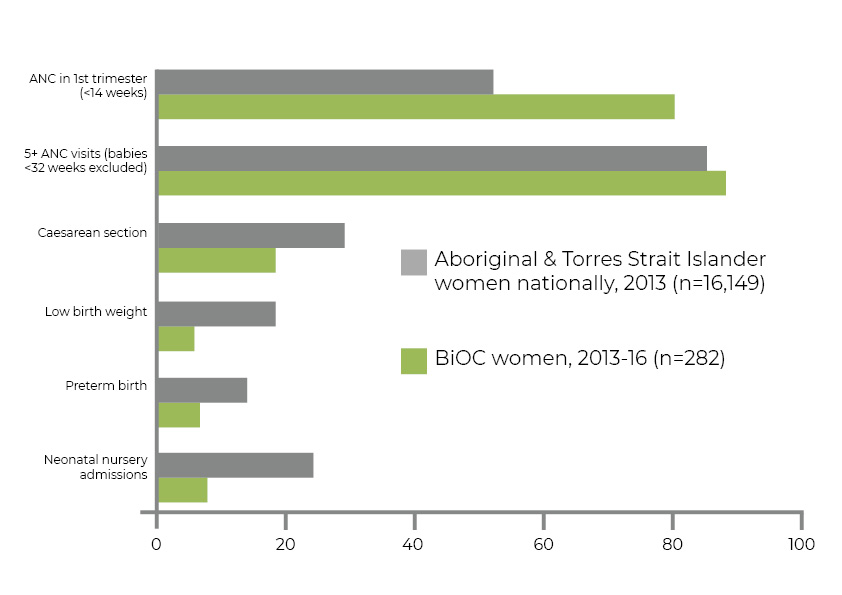
Only 53% of Indigenous mums receive ANC in the first trimester of pregnancy (less than 14 completed weeks) compared to 60% of non-Indigenous mums. Early, high quality ANC helps mums, and their growing bubs, keep strong and deadly.
Too Early, Too Small: Targeting preterm (<37 weeks) birth and low birth weight (<2,500 grms) bubs
Too many babies are born too early (14% vs 8% of non-Indigenous bubs) and too small (12% vs 6%) We want to close this gap because bubs who are born on time and at the right weight are less likely to:
- Spend time away from mum in a neonatal intensive care unit
- Develop a disability
- Develop diabetes, heart disease and kidney disease in adulthood
Too Much, Too Soon: Targeting normal birth
The Lancet Series on mum’s health talks about too much (intervention in birth) too soon being a problem for some high-income countries like Australia. Although sometimes things like inductions (bringing labour on early), epidurals (needle in the back that decreases pain and movement in birth) and caesareans (operation to have bub) can be lifesaving they can also cause harm. A normal birth (no induction, epidural or caesarean) is better for mum (less complications) and better for bub across the lifetime (less diabetes, asthma and obesity in adulthood).
Too Little, Too Short: Targeting breast-feeding
Human breast milk is the best food for human babies. The World Health Organization recommends bubs be breastfed exclusively for six months because of all the health benefits. Mums’ who breastfeed are less likely to get ovarian or breast cancer, diabetes or heart disease. Bubs who receive breast milk are less likely to have gastrointestinal (diarrhoea and vomiting) or respiratory (lung) infections or childhood leukaemia. They are also less likely to be grow up to be obese or get Type 2 diabetes and they are smarter (higher performance on intelligence tests).